With over 100 million Americans living with diabetes or pre-diabetes[note]https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html[/note] and millions more with brewing blood sugar imbalances, having a clear picture of your blood sugar levels is crucial.
And while a fasting glucose test does provide some valuable context, this lab marker can be misleading and doesn’t give you a full picture of how your body is managing sugar over a period of weeks.
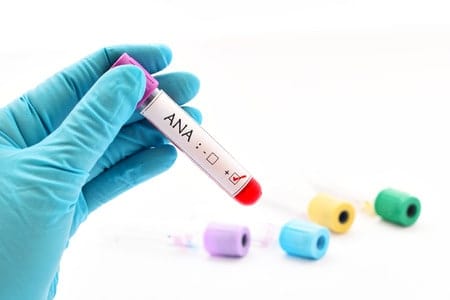
That’s where the Hemoglobin A1c (HbA1c) test comes in handy, and why we include it in our initial membership lab work.
In today’s article, we’ll take a deep dive into the lesser-known consequences of poor blood sugar management, and how the HbA1c test offers us precious clues into the trends and causal factors behind blood sugar imbalances.
Why the HbA1c Test Is Far Superior to Standard Fasting Glucose Testing
When we think of blood sugar issues, most of us immediately think: diabetes.
But, Type 2 diabetes is typically only one advanced consequence of high blood sugar imbalance run amok over a lengthy period of time.
In conventional medical labs, the only test typically offered for blood sugar screening is the fasting glucose test.
This works to an extent to diagnose more advanced cases of blood sugar imbalance and diabetes management.
But, since this test was only designed to measure glucose levels during the fasting period, it doesn’t give a full picture of how a person’s body was handling sugar over a period of days or weeks.
Moreover, it doesn’t provide any predictive insight into trends toward diabetes, prediabetes or other blood sugar handling issues. And prediction is key to prevention when it comes disease. Plus fasting glucose is also highly affected by factors completely outside of diet such as particularly poor sleep the night before.
In functional medicine, and at kNew Health, we want to catch blood sugar issues as early on as possible.
The HbA1c test offers us a window into your last 8-10 weeks of blood sugar handling vs. a one-time glucose test. Plus, it gives us clues into how sugars may be affecting your cells and tissues. HbA1c measures the extent to which hemoglobin in the blood has been affected (“glycosylated’) by blood sugar.
“Optimal/Functional” HbA1c Ranges vs. “Normal”
In functional medicine, we’re always looking beyond “normal” when it comes to lab marker ranges.
Why? Because “normal” doesn’t necessarily equate to optimal if you’re interested in preventing disease—especially when it comes to preventing future blood sugar issues.
Optimal/Functional HbA1c Ranges:
- Optimal Range: less than 5.3
- Less than Optimal/Pre-diabetic stage: 5.4-6.0 (your lab will call this “normal” but, in functional medicine we consider this the concerned-zone)
- Sub-optimal: Anything above 6.0 reveals a problem state with blood sugar control
Individuals who have particularly high or low hemoglobin levels will not be able to rely on HbA1c ranges. Keep in mind too that HbA1c is not the only marker we recommend for assessing blood sugar issues and the insulin resistance that often causes it. But it’s a powerful one to assess for most.
The Health Affects of Chronically High HbA1c
The consequences of sub-optimal or less-than-optimal HbA1C ranges over a period of time include an increased risk of: [note]https://www.ncbi.nlm.nih.gov/pubmed/26577885[/note][note]https://www.ncbi.nlm.nih.gov/pubmed/19229228[/note][note]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265876/[/note]:
- Certain cancers
- Cardiovascular disease
- Stroke
- Diabetes
- Increased annual brain shrinkage
As mentioned above, chronically high HbA1c levels also corrode tissues, blood vessels and your organs most susceptible to glucose.
Some common examples include your optic nerve, your brain, your heart, and your kidneys—which directly correlate to the greater health consequences listed above.
What Causes High HbA1c?
It’s easy (especially in the integrative health world) to place the blame of high HbA1c levels squarely on too much sugar in the diet…
…but that is not always the case folks!
The truth is there are a variety of foods and lifestyle factors that can directly affect your HbA1c levels such as:
- Sleep issues—believe it or not, sleep deprivation is a leading causal factor behind blood sugar imbalances. A recent study showed…
- Stress—chronic stress can really do a number on your blood sugar levels because excessive stress hormones raise blood sugar and can create insulin resistance. For example, a study showed…
- Too many carbs, or too many of the “wrong” carbs—for sure, excessive consumption of sugar and refined carbohydrates can wreak havoc on your blood sugar issues. But that doesn’t mean all carbs will hurt you. “Good carbs” like those found in moderate amounts of whole fruits, vegetables and even sweet potatoes or white potatoes with the skins-on should typically be included in a healthy diet.
- Artificial sweeteners—artificial sweeteners like aspartame, sucralose and saccharin have recently been shown to affect your blood sugar levels.
- Not enough muscle mass/lack of exercise—muscle helps your body regulate blood sugar. Therefore, if you’re lacking in lean muscle mass due to lack of exercise, that could contribute to high HbA1c
How to Lower your HbA1c Levels
Your knew Health Coach will work with you to develop a custom plan, but in general you can easily lower your HbA1c levels by:
- Reducing your intake of refined carbs and sugar—to make this easy, substitute stevia for sugar wherever you can (stevia is a non-artificial plant extract sweetener), cut back on processed foods, and try cutting down to just 1-2 servings of grains a day.
- Increase your protein intake—protein helps stabilize blood sugar while increasing satiety. And while you don’t need to go crazy with this, aim to have a little lean animal or plant-based protein at every meal and snack.
- Get on a regular exercise program—your goal here is not to kill yourself or run a marathon, rather focus on exercises that build muscle mass by challenging you. Burst or interval training, weight training, yoga, and other weight-bearing exercises are excellent for this.
- Work on stress management— believe it or not, this is one of the most profound things you can do to impact your blood sugar levels. Stress-busters include:
- Exercising
- Listening to music
- Journaling
- Spending time with friends
- Laughing
- Meditation
- Spending time in nature
- Getting off your screen more often
- Optimize your sleep—if you’re not getting 7.5-9 hours of sleep a night, your blood sugar will suffer. Some helpful tips to get more zzzzs include:
- Expose yourself to bright morning light (this helps reset your internal clock)
- Stopping caffeine by noon
- Get enough exercise at least 4 hours before bedtime (this will make you tired and help connect body to mind)
- Turning off screens and devices 1-2 hours before bed (otherwise, all that full spectrum light tells your brain to Wake up!)
- Eat dinner earlier (active digestion can often keep people up at night)
- Stick to a bedtime routine (this means you wind down and go to sleep the same way, at around the same time every night)
- Journal out your thoughts, next day’s plans, and worries before bed to clear your mind
- Sleep in a completely dark room to stimulate natural melatonin production
- While we don’t recommend relying on sleep aids, a calming cup of chamomile, valerian, passionflower, or skullcap tea can really help you wind down
How Often to Recheck HbA1c?
Physicians typically recommend patients with type 2 diabetes check their HbA1c every six months to ensure adequate treatment. At kNew Health, we believe in the same vigilance to make sure that your lifestyle changes are giving you the Results you want. If your level falls in the concerned-zone above, we will recommend you check progress at least every 6 months.
From a prevention perspective with optimal levels, we recommend checking HbA1c every year or two. As you’ve learned in this article, many areas of lifestyle choices over time can add up to create insulin resistance and blood sugar imbalances. So it’s best to be empowered and stay on top of your body’s feedback to manage imbalance proactively – before it ever has a chance to become disease.